Researchers from the University of Alberta have uncovered potentially hazardous side effects associated with the popular weight-loss drug Ozempic.
In a study published a month ago by the prestigious Journals of the American College of Cardiology (JACC), the research team led by Jason Dyck, a distinguished pediatrics professor and Canada Research Chair in Molecular Medicine, sought to establish if there were any links between skeletal muscle loss and the use of Ozempic.
By using a sophisticated experimental approach, the researchers conducted trials on mice that simulated dietary conditions similar to those adopted by individuals who use these weight-loss medications.
The results were both fascinating and concerning. Over a mere three-week period, the mice demonstrated an 8.2% reduction in skeletal muscle mass and lean body weight. Perhaps more alarming, the muscle loss was not confined to skeletal muscles as it also extended to cardiac muscles, affecting both obese and lean subjects.
“Given the growing number of people taking this drug who have no cardiovascular disease or who are not classified as obese, we suggest that cardiac structure and function be carefully evaluated in previous and ongoing clinical studies,” the authors of the study asserted.
Using Ozempic Could Result in Compromised Immunity
Contrary to popular belief, muscles are not just responsible for movement and physical strength. They are complex structures that play a critical role in human metabolic health, the performance of their immune system, and physiological functions.
The renowned nutrition expert Carla Prado from the University of Alberta provided critical insights into the implications of muscle loss. She published a paper in The Lancet that emphasized that up to 40% of weight loss could potentially be muscle mass.

This is an alarming percentage that exceeds the outcome of traditional dieting or natural aging.
The long-term consequences of muscle loss are severe. First, they are responsible for creating amino acid reserves that help the body deal with episodes of stress, injury, or illness.
Moreover, they play a key role in managing the body’s level of sugar and are critical to preventing metabolic diseases like diabetes. In addition, they send signals to the immune system through specialized molecules called myokines.
If Ozempic produces muscle loss as researchers seem to be saying, it could mean that the drug could reduce patient’s immunity, increase their susceptibility to infections, and even cripple their wound-healing process.
“If people have been prescribed these drugs, then the benefits should likely far exceed the risks,” Dyck emphasized.
He continued, saying: “However, the growing number of people who may be taking these drugs who do not meet the eligibility criteria and who are not at risk have a different risk-reward calculation that they should be made aware of.”
The research study also suggested that the muscle decline associated with these medications could exacerbate conditions such as sarcopenic obesity. This is a condition characterized by high body fat and low skeletal muscle mass that is known to contribute to adverse health outcomes including increased cardiovascular disease risk and higher mortality rates.
Eli Lilly and Novo Nordisk Have Been Hit With Lawsuits Amid Undisclosed Side-Effects
These new studies are surfacing at a point when the pharmaceutical companies that manufacture these weight-loss drugs are facing multiple lawsuits from patients that experienced complications and adverse side-effects when using semaglutide.
Also read: The Ozempic Lawsuit: Here’s What You Need to Know
Eli Lilly and Novo Nordisk have been hit with legal proceedings that are currently being overseen by US District Judge Karen S. Marston. Their weight-loss drugs Ozepic, Wegovy, and Mounjaro have been linked with incidences of gastroparesis, ischemic bowel syndrome, necrotizing pancreatitis, gallbladder disease, deep vein thrombosis, and pulmonary embolism.
The plaintiffs argue that pharmaceutical manufacturers prioritized financial gains over comprehensive safety disclosures and effectively exposed patients to significant health risks without providing adequate warnings about the potential long-term consequences of ingesting these medications.
GLP-1 Was Used to Treat Diabetes, Then Came Ozempic
The side effects associated with the use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are the core subject of study by medical research at the moment. This substance was developed as a treatment for type 2 diabetes as it helps patients control their blood sugar levels.
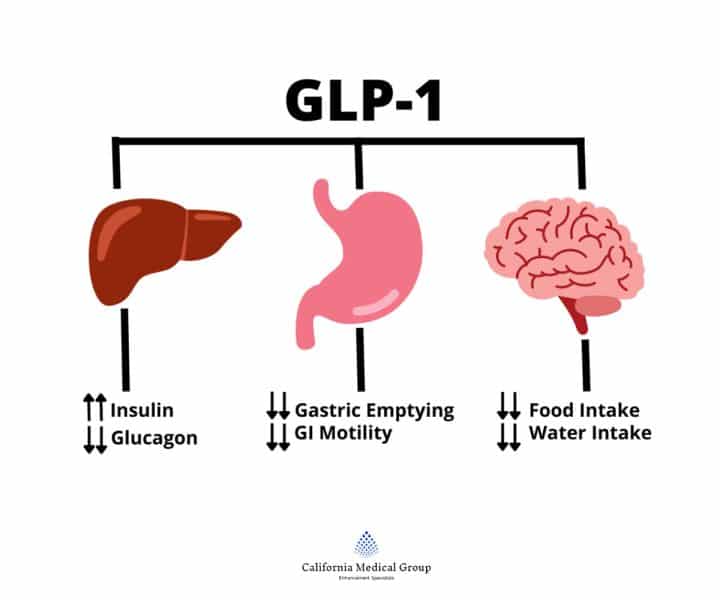
However, semaglutide, the active ingredient of Ozempic and other similar drugs, was considered an innovation in the pharmaceutical industry as it became the evolution of GLP-1 into a weight-loss solution.
The medication’s ability to suppress appetite and modify metabolic processes has made it extraordinarily popular and transcended its initial medical purpose.
In light of these findings, both researchers and medical professionals are urging the public to adopt a measured approach to the use of drugs like Ozempic for weight management purposes.
Also read: Ways to Help You Lose Weight – Scientifically Proven
Nutrition and exercise have been pointed identified as critical components of a balanced approach. Researchers like Prado stress the importance of high-quality protein intake, essential vitamins and minerals, and targeted resistance training.
Protein supplements might also be included in a patient’s diet to ensure that the body receives necessary nutrients while specific exercise regimens can help mitigate the muscle breakdown associated with Ozempic’s intake.
More Studies Are Needed to Assess the Long-Term Consequences of Using Ozempic
The University of Alberta study does not definitively condemn these weight-loss medications but does prompt researchers to study the drug and its side effects further.
The authors emphasize that while no immediate detrimental functional effects were observed in the test subjects, the potential long-term impact of the drug’s use now needs to be carefully assessed.
Jason Dyck and his team strongly recommended a careful evaluation of cardiac structure and function in ongoing and future clinical studies, particularly for individuals without pre-existing cardiovascular conditions or those not clinically classified as obese.
As the scientific and medical communities continue to investigate these complex medications, patients are urged to maintain open and transparent dialogues with healthcare providers.
The study highlights the importance of implementing a personalized approach that carefully weighs potential risks and benefits before prescribing drugs like Ozempic.
